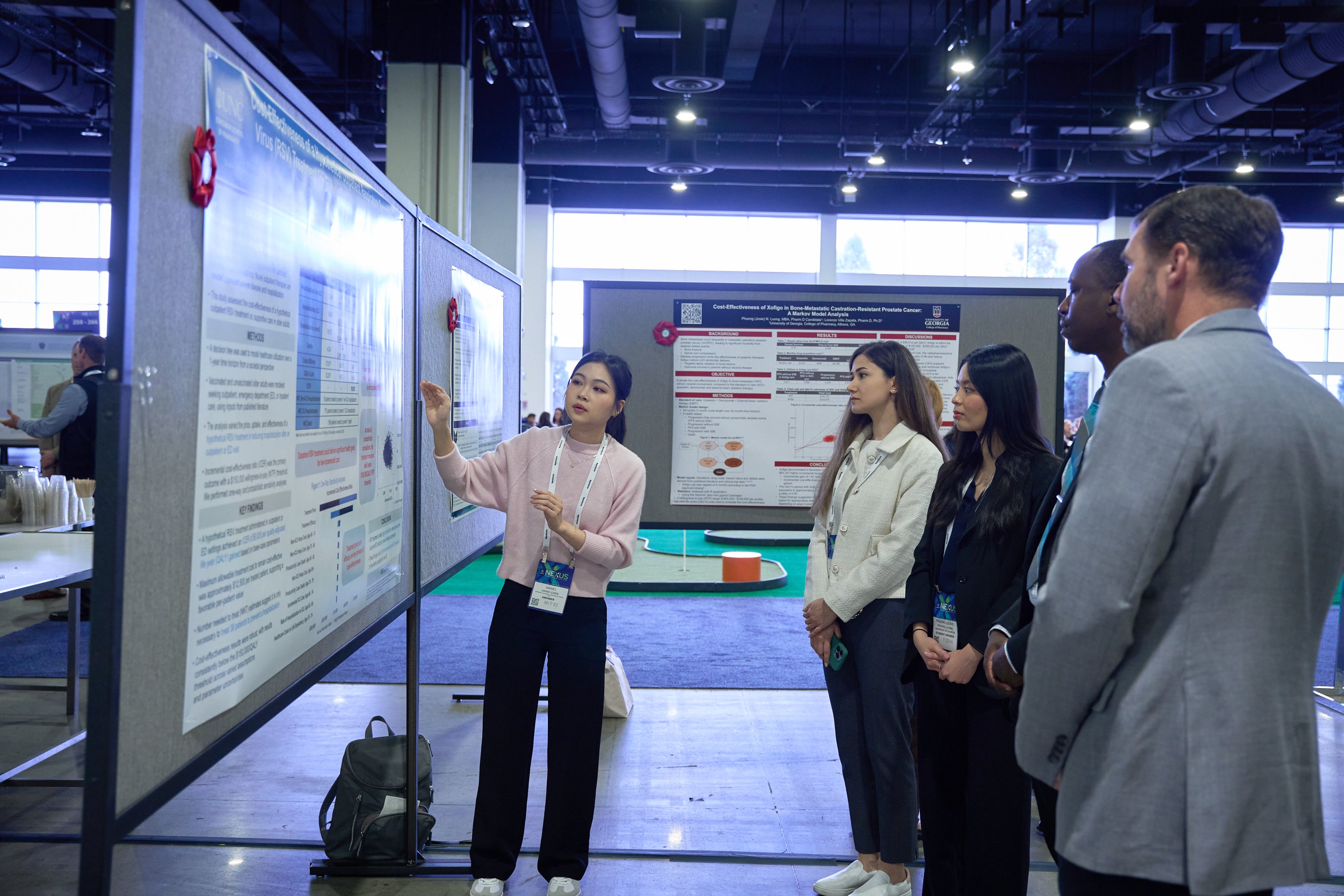
Posters at AMCP 2026 showcase groundbreaking research and real-world insights that are driving the evolution of managed care pharmacy. Featuring 400+ peer-reviewed posters from health plans, PBMs, integrated delivery networks, academia, and pharmaceutical professionals, this year’s posters highlights advances in real-world evidence, outcomes research, health equity, value-based care, and the responsible use of AI and advanced analytics. Attendees can explore practical applications, emerging methodologies, and data-driven strategies that inform formulary decision-making and improve patient outcomes, while engaging directly with the researchers and practitioners behind the work. Whether you’re seeking fresh perspectives or actionable evidence, the AMCP 2026 posters offer an unmatched opportunity to learn from the forefront of the field.
Below is a small sample of posters you will see at AMCP 2026.
Encore
- Efficacy and safety of two rimegepant dosing regimens for the prevention of episodic migraine: a double-blind, placebo-controlled study
- Rimegepant for the prevention of episodic migraine in adults with prior inadequate response to oral preventatives
- A phase 4 randomized double-blind placebo-controlled study of rimegepant for acute treatment of migraine in adults unsuitable for triptan use
- The economic benefit of biosimilars in North America: a targeted literature review
- Systemic inflammation and its association with major adverse cardiovascular events in patients with acute myocardial infarction
- Risk of major atherosclerotic cardiovascular disease events in the United States among individuals with and without prior events
- Clinical and economic burden of adding ezetimibe or PCSK9i therapy in patients with atherosclerotic cardiovascular disease
- Lipid-lowering therapy patterns of high-risk cardiovascular patients without prior myocardial infarction or stroke: VESALIUS-REAL - Results from patients with high-risk diabetes in the US
- Excess cardiovascular events and healthcare resource utilization with lack of lipid lowering therapy in US adults with or at risk of atherosclerotic cardiovascular disease
- Healthcare resource use and costs among US patients are higher after a second ASCVD event than after a first
Professional
- Where You Live Matters: Regional and Racial Disparities in Opioid Treatment for Chronic Noncancer Pain
- Benefit type used by individuals initiating cabotegravir long-acting for human immunodeficiency virus pre-exposure prophylaxis in the United States: Findings from the PrEPFACTS study.
- Breadth of Medicare Part D Preferred Pharmacy Networks, 2019-2025
- Out-of-Pocket (OOP) Cost Burden for Prescription Drugs: Trends and Disparities in Commercial Insurance Design
- Real-World Adherence, Persistence and Switching Patterns of an Adalimumab Biosimilar (ABP 501; Adalimumab-atto) in Patients with Inflammatory Bowel Disease and Other Approved Indications: A Retrospective US Claims Database Analysis
- Real-World Adoption Patterns for Adalimumab Biosimilars: A Comparison of Specialty and Other Channels
- Real-World Switching Patterns after Formulary Changes Related to Adalimumab Biosimilars
- Real-World Treatment Persistence and Switching Patterns Among Biologic Therapies in Psoriatic Arthritis: A Retrospective Cohort Study
- Formulary Barriers to Accessing Finerenone for the Treatment of Chronic Kidney Disease (CKD) and Type 2 Diabetes (T2D)
- Clinical and financial impact of treating heart failure patients with finerenone in hospitals with Medicare alternative payment models
Students & Residents
- Outcomes of colectomy with liposomal bupivacaine
- Medicare Part D Benefit Design Changes Before and After the Inflation Reduction Act
- Characteristics of Medicare beneficiaries reaching the Part D out-of-pocket spending cap in 2025
- Evaluating the Financial and Clinical Impacts of Obesity GLP-1 Formulary Exclusions for Self-Insured Employers in a Group Purchasing Organization
- Investigating the Impact of Removing Xolair (omalizumab) Cross-Benefit Management on Total Cost of Care and Member Outcomes
- Healthcare cost savings from an adaptive medication management program: A retrospective cohort study
- Evaluating the impact of medication policy restrictiveness on net per member per month (PMPM) spending for GLP-1 anti-obesity agents.
- Average Sales Price Erosion of Oncology Biologic Agents Following Biosimilar Entry Into The US Market
- Real-World Uptake of Stelara® Biosimilars at Parity Among Commercial Insured New Starts: A Claims-Based Analysis
- The real-world clinical and economic outcomes of a biosimilar-first formulary strategy within an employer population

